Total Pageviews
Open ended lined cones reduce:
Inherited as an autosomal dominant trait
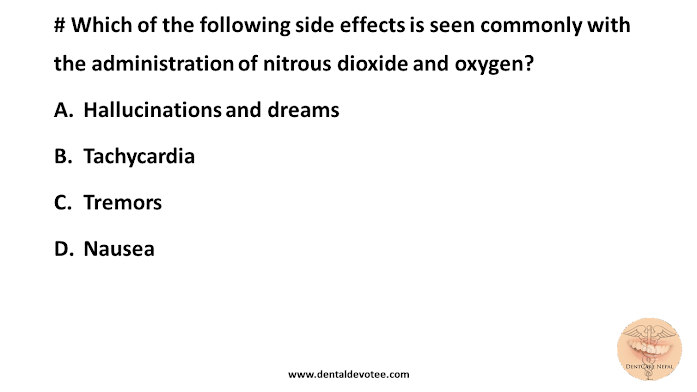
Side effects of Nitrous oxide
MCQs on Diseases of Nerves and Muscles - Oral Pathology
A. Temporal arteritis
B. Neuralgia
C. Neuritis
D. Causalgia
# The latest drug of the choice in the management in trigeminal neuralgia is:
A. valproic acid
B. carbamazepine
C. Diphenyl hydantoin
D. None of the above
# Facial paralysis is tested by:
A. Whistling
B. chewing
C. Protruding the tongue
D. Swallowing
# Which of the following structures are associated with bells palsy:
A. sub mandibular gland
B. Seventh cranial nerve
C. Temporomandibular joint
D. Glosso-pharyngeal nerve
A. VII
B. IX
C. X
D. II
A. it is unilateral
B. it is of throbbing nature
C. it is triggered by touching cheeks, mucosa etc
D. occurs in bouts
A. Pharynx
B. Oropharynx
C. Larynx
D. Nasopharynx
A. Sarcoidosis
B. Multiple sclerosis
C. Trigeminal neuralgia
D. Lupus erythematosus
A. Loss of taste sensation from Ant. 2/3 of tongue
B. Paralysis of orbicularis oculi muscle
C. Loss of innervation to stapedius
D. Loss of lacrimal secretion
A. Excessive lacrimation
B. pain during mandibular movement
C. Stabbing type pain orginate in the tonsillar regions
D. When the jaws are closed the pain subsided
# Which of the following drugs is not effective in case of Trigeminal Neuralgia?
A. Carbamazipine
B. Acetaminophen
C. Phenytoin sodium
D. Baclofen
A. Horner’s syndrome
B. Glossopharyngeal neuralgia
C. Trotter’s syndrome
D. Eagles syndrome
A. Auriculotemporal Neuralgia
B. Trigeminal Neuralgia
C. Sphenopalatine Neuralgia
D. Glossopharyngeal Neuralgia
A. Phenytoin
B. Gabapentin
C. Baclofen
D. All of the above
# Which of the following Orofacial pain is not associated with vascular origin?
A. Cluster headache
B. Giant cell arteritis
C. Anaesthesia dolorosa
D. Chronic paroxysmal hemicrania
A. burning sensations in mouth
B. excessive salivation
C. Glossodynia
D. Dysphagia
# An attack of cluster headache can be aborted by:
A. Morphine administration
B. Breathing oxygen
C. Aspirin administration
D. Sublingual nitroglycerine administration
A. Oral lichen planus
B. Oral submucous fibrosis
C. Aphthous stomatitis
D. No detectable oral disease
# In an acute attack of migraine, the during of choice:
B. Methysergide
C. Propranolol
D. Caffeine
A. Progressive systemic sclerosis
B. Tetanus
C. Multiple sclerosis
D. Osteomalacia
# A patient shows inability to close the right corner of the mouth is most probably suffering form:
A. Myasthenia gravis
B. Bell’s palsy
C. TMJ dysfunction syndrome
D. Multiple sclerosis
# Bell’s palsy is triggered by:
A. Exposure to cold
B. Tooth extraction
C. Local and systemic infection
D. Any of the above
# The following site is the common involvement in case of Myositis ossificans:
A. Massetor
B. Hyoglossus
C. Stylohyoid
D. Lateral pterygoid
# Trigeminal neuralgia:
A. Does not disturb the patient during sleep
B. Can be treated with NSAID’s
C. Always bilateral in distribution
D. Is a hereditary condition
# Carbamazepine has been utilized to successfully diminish attacks in trigeminal neuralgia. During this therapy which of the following is indicated:
A. Clinical observation only
B. Clinical observation and complete blood and platelet counts prior to and at frequent intervals during therapy
C. No monitoring
D. Complete blood investigation only if adverse symptoms arise
# Which syndrome consists of flushing, warmness and perspiration over the cheek and pinna of the ear on the side following the ingestion of highly seasoned food?
A. Fanconi’s
B. Auriculotemporal
C. Horner’s
D. Cushing's
# Facial pain due to elongated styloid process is called?
B. Tic doulourex
C. Eagle’s syndrome
D. Reiter’s syndrome
# A neuralgia with trigger zones in the oropharynx and pain in the ear pharynx, nasopharynx, tonsils and posterior tongue is most likely:
A. Trigeminal neuralgia
B. Bell’s palsy
C. Glossopharyngeal neuralgia
D. Sphenopalatine neuralgia
# Easy fatigability of muscles seen in:
A. Epilepsy
B. MPDS
C. Myasthenia gravis
D. Cerebral palsy
A. Red
B. Yellow
C. White
D. Blue
A. Submandibular salivary gland
B. Parotid gland
C. sublingual salivary gland
D. TMJ
A. Ptosis
B. Anhydrosis
C. Flushing
D. Mydriasis
# Trigeminal neuralgia (tic doulourex) is characterized by:
A. Paralysis of one side of the face
B. Uncontrollable twitching of muscles
C. Sharp, excruciating pain of short duration
D. Prolonged episodes of plain on one side of the face
# TENS therapy is useful in:
A. MPDS
B. Trigeminal neuralgia
C. Facial palsy
D. Neurosis
# Bell’s Palsy is characterized by:
A. Bilateral involvement of the side of the face
B. Inability to whistle
C. No loss of muscular control
D. Closing of the eyes
Dental Management of Hyperventilation
Dental management of Medical compromised patient _ Hyperventilation
Dental Management of Hyperventilation
Hyperventilation is an increase in the rate or depth of breathing that results in a change in the blood chemistry and usually occurs as a result of anxiety. The dental office is an anxious setting for most people, which is why hyperventilation is a very common emergency seen there.
The most common cause of hyperventilation is anxiety. Although not as common, hyperventilation also may be caused by certain physical conditions, emotional upset, or stress. Children usually cry or scream when frightened, which expresses their fears and prevents hyperventilation from occurring.
Carbon dioxide in the blood automatically triggers the breathing reflex and stimulates respiration. In this way it helps control the breathing process automatically. A person who begins to hyperventilate increases the depth and rate of respirations much like an athlete who has performed strenuous exercise. By increasing respirations, the person exhales a large amount of carbon dioxide. In the athlete, the exercised muscles release carbon dioxide into the blood, which replenishes the excess given off by the rapid breathing. Because dental patients are motionless, however, they have no way of replenishing the carbon dioxide being exhaled. As a result patients can suffer from a lack of carbon dioxide and have difficulty breathing. When there is a lack of carbon dioxide, the patient must consciously work to inhale and exhale.
Signs and Symptoms of Hyperventilation
- Nervousness
- Increase in rate of respirations
- Feeling of suffocation
- Tightness in chest
- Dizziness
- Tingling in extremities
Treatment for Hyperventilation
- Stop dental treatment
- Position the patient in a upright position
- Calm the patient by describing the situation and ask the patient to hold his or her breath “Tell the patient to inhale and hold his or her breath for several seconds before exhaling. This procedure will help increase the level of carbon dioxide.”
- Have the patient breathe into a paper bag to increase carbon dioxide in the bloodstream. “Never administer oxygen to a hyperventilating patient. Remember, this patient already has too much oxygen and too little carbon dioxide”
- Administer drug therapy to reduce anxiety such Diazepam (Valium) (only if necessary, as a last resort)
Dental Management of Asthmatic Patient
Dental management of Medically compromised patient _ Asthma
Dental Management of Asthmatic Patient
Asthma is a respiratory disease that causes reversible airway obstruction and a reduced ability to expire or completely empty the lungs of gases. Inflammation is a component of the disease process and results in increased mucous secretions in the lungs and swelling in the bronchioles.
Clinical Manifestations include:
1. Cough
2. Shortness of breath
3. Chest tightness
4. Wheezing.
5. Increased heart rate
6. Nervousness
7. Sweating
The most common form, called extrinsic asthma, develops as a result of allergy to environmental pollutants. It generally occurs during childhood and may or may not extend into adult years.
A second type of asthma is intrinsic asthma, or infectious asthma, is A non-allergic form of asthma usually first occurring later in life that tends to be chronic and persistent rather than episodic , most often seen in patients older than age 35. Unlike the extrinsic asthma patient, this patient may exhibit a chronic cough with sputum production between attacks. Intrinsic asthma usually occurs as a result of some type of bronchial infection.
Oral Complications associated with asthma medications include dry mouth, candidiasis, and an increased dental caries rate.
TREATMENT (Dental Management of Asthmatic Patient)
1. Stop all dental treatment. Be sure to remove all materials and instruments from the patient’s mouth.
2. Position the patient. Raise the patient upright; since the patient will be struggling for air, it will be easier for the patient to breathe if seated upright.
3. Use a bronchodilator. The patient’s bronchodilator should be placed within easy reach in case an attack occurs. If an attack does take place, allow the patient to administer the bronchodilator; patients know what their usual dose involves . The bronchodilator is an aerosol medication that usually includes epinephrine, which relaxes the bronchioles and makes it easier for the patient to breathe.
4. Administer oxygen.
5. Administer epinephrine or another drug intravenously it may be necessary, if the bronchodilator does not relieve the attack.
MCQs on Instruments Used in Oral Surgery
A. Adjacent tooth is the fulcrum
B. Tooth is isolated
C. Interdental bone is fulcrum
D. Adjacent tooth is not to be extracted
# Most of the elevators used in exodontias works on the principle
A. Class I lever
B. Class II lever
C. Class III lever
D. Wheel and axle
Featured Post
Dental MCQs - Multiple Choice Questions in Dentistry
SELECT THE TOPIC YOU WANT TO PRACTICE. # LOK SEWA AAYOG PAST QUESTIONS Medical Entrance Preparation MCQs # Digestive System and Nutriti...

Popular Posts
-
SELECT THE TOPIC YOU WANT TO PRACTICE. # LOK SEWA AAYOG PAST QUESTIONS Medical Entrance Preparation MCQs # Digestive System and Nutriti...
-
NOTE: If you cannot find any books here in the list below, You can search yourself in the Library Genesis Website Database. DISCLAIMER: We ...
-
# Class IV Kennedy classification is: A. Bilateral edentulous area located posterior to the remaining natural teeth B. Unilateral ed...
-
# Faulty registration of occlusion cannot be directly attributed to: A. Viscosity B. pain in the muscles of mastication C....
-
# Which is the immediate danger to a patient with severe facial injuries? A. Bleeding B. Associated fracture spine C. Infection ...
-
NOTE: It has been proved that you will retain more of what you study if you study first and then test yourself immediately. For that, Fir...