Surgical Management of Oral Leukoplakia: A Case of Laser Excision
Dr. Soni Bista,1
Dr. Rebicca Ranjit,2
Dr. Suraksha Subedi3
1,3Department of Periodontology and Oral Implantology, Gandaki Medical College, Kaski, Nepal
Correspondence : Dr. Soni Bista. Email: sonibista1234@gmail.com
ABSTRACT
Oral leukoplakia is the most frequent potentially malignant disorder of the oral mucosa which requires
definite treatment. A wide variety of medical and surgical treatment modalities have been endeavoured
with varying degrees of success. Among various surgical treatments, laser techniques have helped
improve surgical approaches and ultimate control of leukoplakia. The present case reports homogenous
leukoplakia in an adult male treated successfully with diode laser and followed up for six months without any complications and recurrence. Thus, the application of diode laser is safe and can be effectively used as a good substitute for the management of oral leukoplakia.
Keywords: Diode lasers; laser therapy; oral mucosa; oral leukoplakia.
INTRODUCTION
The term leukoplakia is recognized as white patches of questionable risk having excluded known diseases or disorders that carry no increased risk for cancer.1 The cause is multifactorial including tobacco or areca nut use, alcohol abuse, human papilloma virus, fungal infections, chronic
trauma, and nutritional deficiency.2
Different modalities for its management includes medical therapy (antioxidants, Vitamin A), surgical therapy using scalpel, electrocautery, and laser.3 Surgical excision done by soft tissue diode laser have shown beneficial role in the treatment of the lesion.4 This paper reports a case of oral leukoplakia treated successfully with the application of diode laser.
CASE REPORT
An adult male aged 60 years reported to the Department of Periodontology and Oral Implantology of Universal College of Medical Sciences, Bhairahawa, Rupandehi, Nepal with a chief complaint of white patches on his right lower back gum region for two years. The patient’s medical history and family history were non-contributory. He had the habit of smoking tobacco, one pack of bidi (25 bidis) per day for 10 years. On extraoral examination, there were no significant findings.
On intraoral examination, white plaques were appreciated on right lower buccal gingiva of the posterior teeth extending from the first premolar to the second molar involving their marginal, attached and papillary gingiva (Figure 1). The lesion was non-scrappable, had firm consistency, diffused margins, wrinkled surface, crack-mud appearance measuring approximately 7x4 cm2
with normal
surrounding mucosa. Class II Gingival recession
was observed in relation to #46 (according to two-digit numbering system). Furthermore, stain and
calculus were present in all teeth. The provisional
diagnosis was made as homologous leukoplakia on
right buccal gingiva in relation to #45, #46, and #47
because at clinical examination a predominantly
white lesion was appreciated which cannot be
clearly diagnosed as any other disease or disorder
of the oral mucosa.

Following an initial examination and treatment
planning discussion, the patient underwent
nonsurgical periodontal therapy including scaling
and root planing with oral hygiene instructions. He
was given strict advice for complete cessation of
the habit of smoking tobacco and prescribed with
Tablet BNM forte (Lycopene, Meobalamin, Omega
three with multivitamin) twice daily for a month.
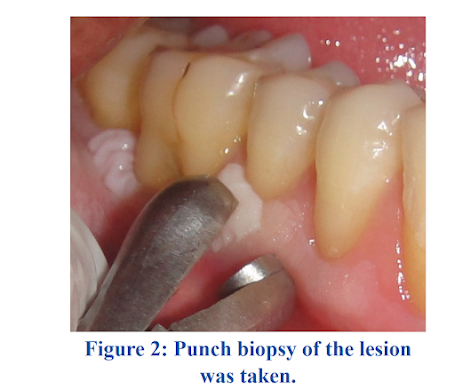
Meanwhile, a punch biopsy with a diameter of
0.5 cm (involved and normal tissue) of the lesion
from marginal and attached gingiva in relation to
#45 was sent for histopathological examination
as it is mandatory to rule out any malignancy
(Figure 2). The histopathological analysis revealed
a hyperkeratinised stratified squamous epithelium
with mild dysplasia (Figure 3). On the basis of
clinical presentation and histopathological reports,
a definite diagnosis of Homogenous Leukoplakia
with mild dysplasia on buccal gingiva in relation
to #45, #46, and #47 was made. The patient did not
respond to conservative medical management with
multivitamins, multiminerals, and antioxidants (Tablet BNM forte) even after a month of followups, so he was advised for complete excision of the
lesion using a diode laser. A complete haemogram
was done which depicted values within normal
limits. Written informed consent was taken from
patient.
On the day of surgery, a complete protocol for
surgical preparation was followed. The patient
was asked to do a presurgical mouthrinse using 2
ml of 0.2% chlorhexidine diluted solution, and 5%
povidone-iodine solution (Betadine) was used to
perform extraoral antisepsis. Right inferior alveolar
nerve block using 2% lignocaine with adrenaline
1:200,000 was administered. Safety measures were
taken for the operator, patient, and assistants by
wearing the recommended laser protective eyewear.
High-speed suction and surgical masks were used to
prevent infection from the laser plume. Diode laser
(iLase™) emitting 940 nm was used for excision
where a preset value was adjusted: power of 3.00
W, pulsed contact mode, continuous pulse duration,
and pulse interval of 1.00 ms. Blunt end of the
probe was used to check for objective symptoms.
After the area was anaesthetised, the excision of
the lesion in the right lower posterior gingiva and
buccal mucosa was carried out using a bendable
laser tip with a diameter of 300 mm (Figure 4).
After excision, the surgical site was wiped off
with a cotton pellets soaked in normal saline. The
operated site was then protected with periodontal
dressing (COE–PAKTM GC America) (Figure 5, 6).
The entire procedure was painless with no bleeding
and lesser intraoperative time.


Post-surgical instructions were given with the
prescription of analgesics (Ibuprofen 200 mg,
if needed) and warm saline rinse (three to four
times/day for two weeks). To minimise traumatic
injury to the wound, mechanical tooth cleaning
was restricted to the surgical site for the first week.
The patient was recalled immediately after a week
for removal of periodontal dressing then after two
weeks and six months for revaluation (Figure 7, 8).
No complication without recurrence was observed
at follow-ups.
DISCUSSION
The management protocol for leukoplakia should
be based on grade of dysplasia, size, and location
of the lesion; however, local factors such as trauma
and adverse habits such as using tobacco should be
controlled. Both non-surgical and surgical treatment
modalities can be applied with varying success. In
non-surgical methods, anti-inflammatory agents,
carotenoids, retinoids, antimycotic agents, and
cytotoxic agents can be used topically. Chemopreventive agents such as vitamins (A, C, E),
fenretinide (Vitamin A analogue), carotenoids (beta
carotene, lycopene), green tea, curcumin are also
beneficial. They play a vital role during the early
healing of the lesion but they will appear once the
patient stops taking the supplements. Researchers
have found it to be less convincing and possessing
a longer duration of treatment. In the present case,
combination of multivitamins, multiminerals, and
antioxidants drug was prescribed to the patient for a
month, but it did not show any effect. Thus, surgical
excision was opted as an appropriate treatment for
the case.
Surgical treatment can be carried out using scalpel,
cryotherapy, electrocautery, and laser, but will not
prevent all premalignant lesions from undergoing
malignant transformation, which can be explained
by the genetic defects even in the normal appearing
mucosa surrounding the excised lesion (field
cancerisation).4
Surgical excision of lesions using laser offers
several advantages over scalpel excision which
includes bloodless surgical and postsurgical events;
the ability to precisely coagulate, vaporise, or cut
tissue; minimal swelling and scarring; reduction
of surgical time, postsurgical pain with high
patient acceptance.5
Previous study has evidenced
promising results using lasers in the excision of oral
leukoplakia.6
The diode laser is not indicated as the main laser for soft tissue surgery, but its versatility
of use led us to choose it for the study. In the present
case, the patient reported minimal intraoperative and
post-operative pain and discomfort. These results are
similar to the findings of Mohan et al., who reported
minimal post-operative pain and discomfort.7
The
wound healing was also satisfactory similar to
the previous study.7
Histologically, laser-created
wounds heal more quickly and produce less scar
tissue than conventional scalpel surgery,8
although
contrary evidence also exists.9
In the present case,
the patient did not show any signs of recurrence
in six months’ follow-up. This was similar to the
findings of a study conducted in Natekar et al.,10 the
patients in their study showed no sign of recurrence
on six months’ follow-up. Although laser has many
advantages, it requires some precautions during and
after irradiation such as using protective eyewear,
high-speed evacuation, and a properly trained
operator as an important part of laser safety.
Thus, the main purpose of treating oral leukoplakia
is to prevent transformation into a malignant form
as the patients are mostly asymptomatic. Diode
laser provides an effective technique with marked
clinical improvement and high degree of patient
acceptance in the management of oral leukoplakia.
Conflict of interest: None.
REFERENCES
1. Warnakulasuriya S, Johnson NW, Van der Waal I. Nomenclature and classification of potentially malignant disorders of the oral mucosa. J Oral Pathol Med. 2007;36(10):575-80. [
PubMed |
Full Text |
DOI]
2. Goyal D, Goyal P, Singh HP, Verma C. An update on precancerous lesions of oral cavity. Int J Med Dent Sci. 2013;2(1):70-5. [
Full Text |
DOI]
3. Lodi G, Franchini R, Warnakulasuriya S, Varoni EM, Sardella A, Kerr AR, et al. Interventions for treating oral leukoplakia to prevent oral cancer. Cochrane Database Syst Rev. 2016;7:CD001829.[
PubMed |
Full Text |
DOI]
4. Tatu R, Shah K, Palan S, Brahmakshatriy H, Patel R. Laser excision of labial leukoplakia with diode laser: A case report. Indian Journal of Research and Reports in Medical Sciences. 2013;3(4):64-6. [
Full Text]
5. Bista S, Adhikari K, Saimbi CS, Agrahari B. Comparison of patient perceptions with diode laser and scalpel technique for frenectomy. J Nepal Soc Periodontol. 2018;2(1):6-8. [
Full Text]
6. Gupta P, Thakur J, David CM. Excision of oral leukoplakia using 970 nm diode laser. Int J Adv Integ Med Sci. 2017;13(8):208-11. [
Full Text]
7. Mohan R, Sunil MK, Raina A, Krishna K, Basu M, Khan T. Diode laser therapy of homogenous leukoplakia- A clinical study. TMU J Dent. 2017;4(3):90-2. [
Full Text]
8. Bista S, Adhikari K, Saimbi CS, Agrahari B. Diode laser for lingual frenectomy. J Dent Lasers. 2018;12:74-6. [
Full Text |
DOI]
9. Buell BR, Schuller DE. Comparison of tensile strength in CO2 laser and scalpel skin incisions. Arch Otolaryngol. 1983;109:4657. [
PubMed |
DOI]
10. Natekar M, Raghuveer HP, Rayapati DK, Shobha ES, Prashanth NT, Rangan V, et al. A comparative evaluation: Oral leukoplakia surgical management using diode laser, CO2 laser, and cryosurgery. J Clin Exp Dent. 2017;9(6):e779-84. [
PubMed |
Full Text |
DOI]
Published in: JNDA | Vol. 22 No. 1 Issue 34 Jan-Jun 2022